CivicMeter surveyed 27 epidemiologists from institutions such as the University of Iowa, Emory University, UNC, University of Massachusetts and others.
Our survey focused on two top-of-mind areas: The risks associated with reopening and traveling; and COVID-19 data quality. We also asked experts who did not participate in the survey to weigh in on the final results.
Re-opening and Travel Risks
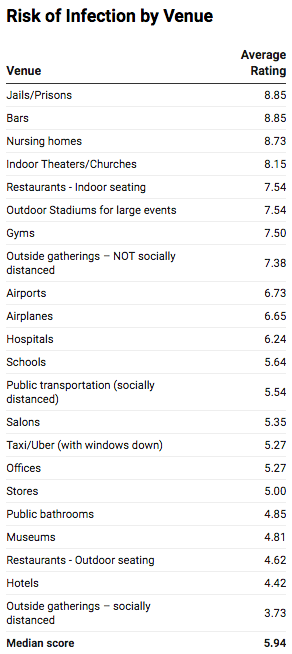
Question #1: On a scale of 1-10, rate the risk of contracting COVID-19 at each venue in the United States. (1 = lowest risk; 10 = highest risk)
WHY WE ASKED: As lockdowns are lifted and states reopen, which venues are safest? All else being equal, which are the highest risk?
THE RESULTS:
The experts cautioned that truly weighing the risk of different locations depends on a variety of factors, including the prevalence of infection in the area, the state and local guidelines and whether they’re being followed, as well as accommodations being made by individual businesses.
EXPERT REACTION:
Professor of Preventive Medicine and Infectious Diseases at Vanderbilt University Medical Center:
“Bars have become notorious as sources of COVID spread. They are almost always indoors. People are there for prolonged periods of time, very close together, they’re unmasked because they’re drinking and talking. And that’s the sine qua non for spread of a respiratory virus.”
“Hotels certainly haven’t been mentioned as a high risk place. If you think about hotels, you have a lot of control over your own circumstances. You check in, you’re distanced from the check-in person. Both people are hopefully masked. You’re not at check in very long. You go up to your room in an elevator alone, and you go directly to your room, where you’re often alone. Pretty safe.”
Associate Professor of Epidemiology, Rollins School of Public Health at Emory University:
“I think a bar is about the utmost unsafe place. My work is with prisons and jails, that’s where I do all my research. I think in theory it’s possible for jails and prisons to be fairly safe, if they have adequate resources for screening individuals coming in (and there are some jails that do); that it can be safer than a bar. I think a bar is the most unsafe place, and that’s after having worked at a lot of prisons and jails.
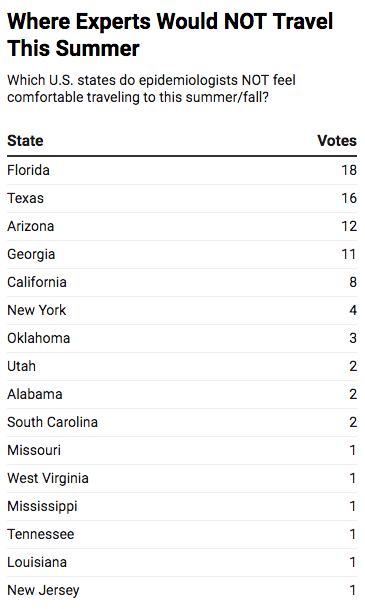
Question #2: Which U.S. states would you be comfortable traveling to this summer/fall? Which U.S. states would you NOT be comfortable traveling to this summer/fall?
WHY WE ASKED: We were interested to learn where epidemiologists are comfortable vacationing this summer/fall. Which states do experts feel comfortable traveling to this summer, and which ones are they avoiding?
THE RESULTS:
The experts cautioned that risk levels can change dramatically depending on many factors, including where in a state you’re traveling to; how you’re getting there (flying vs driving); and where you’re staying (hotel vs remote cabin vs. busy resort).
Data Quality
Question #3: On a scale of 1-10, rate the quality and trustworthiness of COVID-19 data from each country. (1 = lowest quality; 10 = highest quality)
WHY WE ASKED: The pandemic is generating enormous amounts of data. But experts trust the data coming out of some countries more than others. Which numbers are more trustworthy according to epidemiologists?
THE RESULTS:
EXPERT REACTION:
Assistant Professor of Epidemiology and Biostatistics, Drexel University Dornsife School of Public Health:
“South Korea has an excellent public health program and an expansive public health workforce. Early on they were able to collect high quality data on their COVID-19 outbreak through their contact tracing efforts. Germany has a similar story. Early on they had excellent contact tracing efforts in place and were aggressive in their shut down mandates and have been quick to shut down regions again when new cases flare back up.”
“It is understandable that scientists wouldn’t trust data out of Brazil or Russia. Both have authoritarian regimes who have denied that COVID-19 is a substantial health risk. […] There is a general mistrust of data from China owing to China’s past handling of similar situations. However, China worked very close with WHO very early on in the course of the outbreak. I was following the numbers out of China at a very granular level throughout January and February and the epidemiologic characteristics have held true in the other national contexts we’ve seen. I understand that American intelligence believes that the data are untrustworthy, but when I look at it, I see patterns that emerge time and again with this epidemic that if China were manipulating their numbers wouldn’t be there.”
Associate Professor, Division of Health Policy and Management, University of Minnesota School of Public Health
“Countries that are highly ranked also seem to be those countries that implemented robust testing and contact tracing programs and were able to get their epidemics under control (South Korea, Germany). Countries where the epidemic has become political, where leaders are downplaying the severity, where messaging has been inconsistent, and/or where there are contradictory narratives seem to be the ones ranked as less trustworthy (e.g., Brazil, Mexico).”
Associate Professor of Epidemiology, Rollins School of Public Health at Emory University:
“The articles I’ve seen [from Germany and South Korea] have been very high quality articles. I’ve been very interested in how often people have tried to culture the virus, and there are papers from Germans and South Koreans where they give not only the PCR data but also the culture data. And I think that really helps one understand whether or not the PCR represents viable virus.”
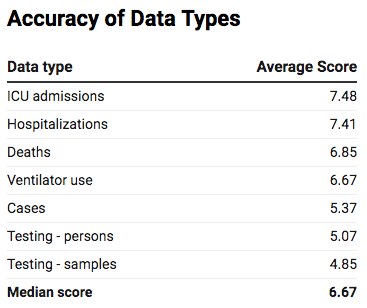
Question #4: On a scale of 1-10, rate the quality of each type of data produced by the United States on average — ignoring best and worst outlier jurisdictions for data reporting (1 = lowest quality; 10 = highest quality)
WHY WE ASKED: Are all types of COVID-19 data of equal quality? Which types of data do experts believe is more accurate on average?
THE RESULTS:
EXPERT REACTION:Assistant Professor of Epidemiology and Biostatistics, Drexel University Dornsife School of Public Health:
“While the trend in testing data is fairly stable (despite increases in testing over time), they still provide a good enough signal of the epidemic trajectory. It would be better if we had hard data from contact tracing, but it doesn’t seem like we’re there yet. All-in-all, from a data perspective our situation in the United States is “just ok”. It could be a lot better and it could be a lot worse.”
“Many of those working with COVID-19 data [in the U.S.] are using data collected from State Health Departments. As a result, we don’t always have comparable measures. For example, some states are providing data on new hospital admissions (incident hospitalizations) while others are reporting concurrent hospitalizations (the number of people hospitalized with COVID-19 on a given day) or cumulative hospitalizations (the total number of people hospitalized). Relatedly, with respect to test results, some locations are reporting cases based on test date and some are reporting based on report date.”
Associate Professor, Division of Health Policy and Management, University of Minnesota School of Public Health
“Since there is so much testing within hospitals and particularly among critically ill patients, it seems reasonable to think that there are very few COVID-19 infections in the ICU that remain unidentified. Same with hospitalizations, but you could imagine testing might be slightly less universal. Deaths are the next most “complete” type of data since many deaths occur in the ICU and hospital. However, if someone dies before they can be tested, they generally won’t be counted (even if they are highly suspected of having died of COVID-19). Some states are reporting “suspected” COVID-19 deaths though. Also, if someone dies outside a healthcare setting and were never tested, they also won’t be counted. As for case data, it’s so dependent on who gets tested and the availability of testing, both of which vary by state / jurisdiction and vary over time.”
Assistant Research Professor, Drexel University Dornsife School of Public Health:
“There have been a host of issues with testing since the first assays became available, coupled with challenges in the roll out including messaging to the public, that I am not surprised testing was ranked lowest. However, this is not to say that these data do not have value — imperfect data is better than no data — and methods that I have helped develop are becoming available with how to use these imperfect data. Some things are more “objective” and easier to identify: hospital admission, being in an ICU, being on a ventilator. Deaths are always challenging given how death certificates can be coded. It is shocking to me that this far into the pandemic, we still are struggling to identify cases accurately.”
ABOUT CIVICMETER:
CivicMeter is a nonprofit journalism outlet focusing on data and measurement in government and public policy. Our work has appeared in or been cited by NPR, Political Wire, New York magazine, and local papers.